AI - Digital Watch
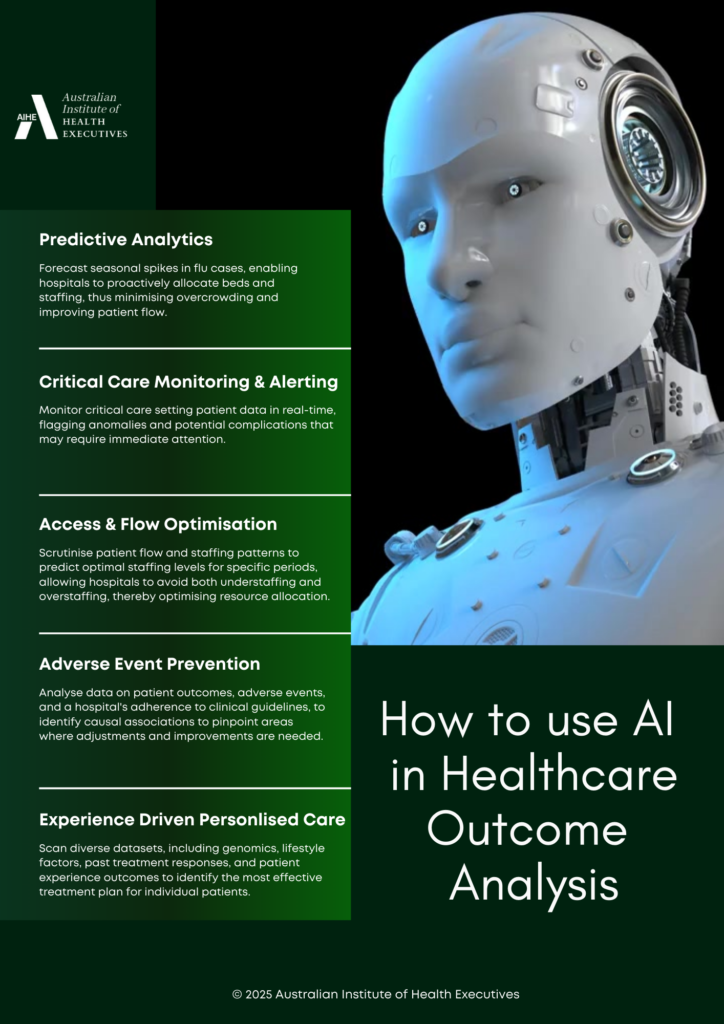
The ability of AI algorithms to process huge amounts of healthcare outcome data, identify subtle patterns and trends that humans might miss, and make accurate predictions offers unprecedented opportunities for improving patient care, advancing precision medicine and optimising healthcare resource allocation.
While this immense potential of AI in healthcare outcome analysis is clear, challenges of course, remain. Data privacy and security concerns, ensuring algorithmic transparency and robustness, and addressing biases in datasets are important considerations in this space.
Stay up to date with curated insights and expert analysis of the healthcare leadership industry. Contact AIHE to access our suite of new CPD programs.
Real-world applications of AI in Healthcare Intelligence
It is no great surprise that attempts towards integrating artificial intelligence within healthcare is rapidly progressing, and increasingly moving beyond theory into practical application. We catalogue some of the impactful real-world applications currently being used within healthcare.
These real-world implementations are demonstrative of the multidirectional expansion, versatility and applicability of AI.
Apart from relegating AI to routine, administrative or automated tasks, using AI to enhance human cognitive elements such as analytical, creative and predictive capability of clinicians and healthcare workers can yield far greater benefit in healthcare. We should be shifting our perspectives to allow for the harnessing AI’s capabilities to work alongside human intelligence in creative and analytical roles, and to more effectively integrate human and machine thinking for enhanced application.
In imaging diagnostics for example, humans and AI both learn by recognising patterns. By pairing AI capabilities alongside clinician capabilities, we can enhance the learning curve of clinicians, helping them to achieve expert proficiency and higher accuracy rates more quickly.
As these areas continue to evolve, it is important for healthcare leaders to understand the benefits, risks and implications of these advancements, including their unanticipated consequences.
In order to maintain high quality, efficient and patient centred care, real-world application of AI and it’s integration within existing healthcare governance processes, must be undertaken with a solid understanding of its limitations and biases. Rigorous testing, validation and a nuanced strategic approach is needed in facilitating safe delivery of AI enhanced human expertise and decision making.
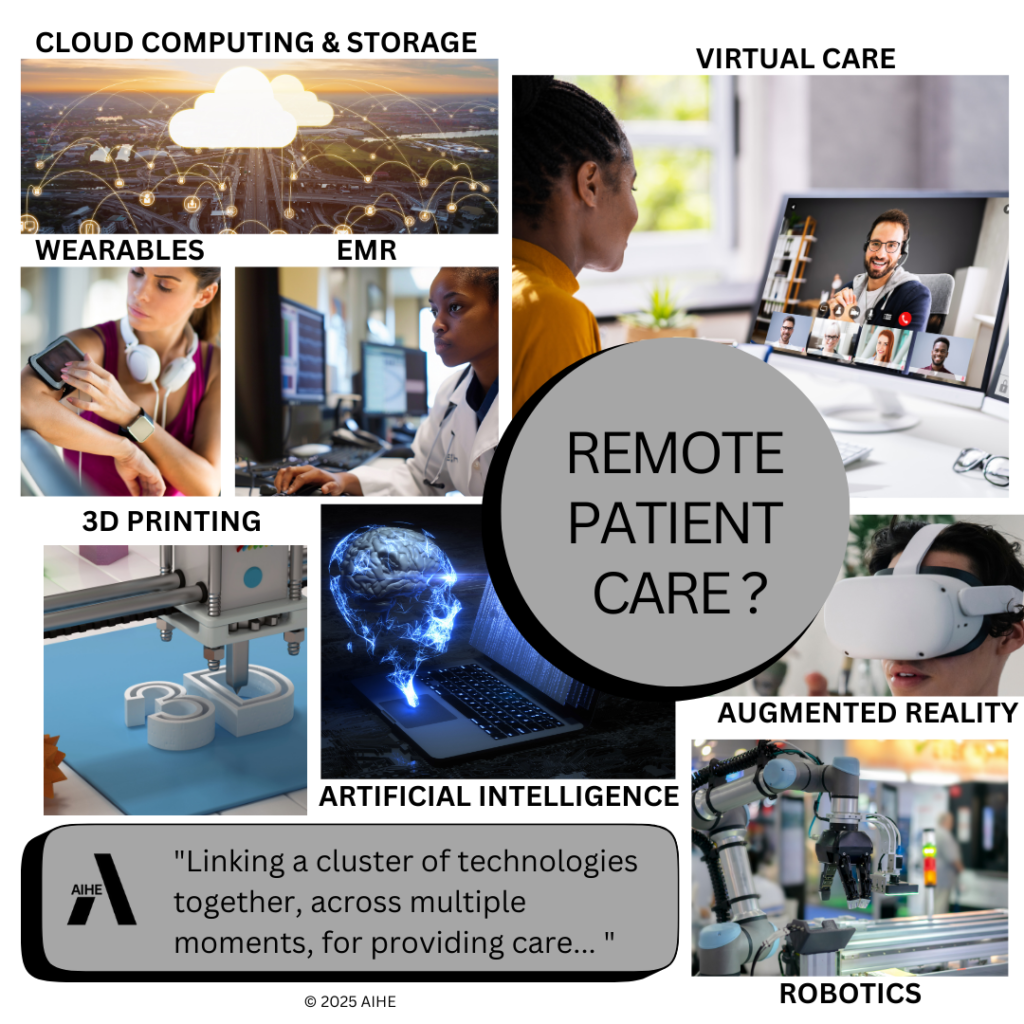
The weathered old house stood on a quiet stretch of road in the forgotten small town, its windows looking longingly out at a world that had long passed it by. Inside sat Mr Brown, in his well-loved armchair, the glow of a new laptop illuminating his wrinkled face in shades of whites and blues. He wasn’t seeing the peeling wallpaper or the worn furniture, he was connected virtually to the medical centre of Dr. Elias, many miles away in the city.
It’s true that he had resisted “remote care” and “telehealth” at first. That was because he had longed for the familiar, the smell of antiseptic in the small dispensary, the knowing look in Dr Bernard’s patient eyes, the reassuring touch on his shoulder as he saw him out after a consult. But Dr. Bernard was long gone now, lost to the relentless tides of time. Dr Elias was his only lifeline now, a stranger separated by screens and algorithms, and yet somehow there for him.
The EMR which was accessible through the “cloud”, held Mr Brown’s life story, his every ache and illness carefully recorded and analysed by AI. His vital signs were now being monitored in real-time and Dr Elias was able to adjust his medication with a timely precision that surprised even an old codger like him.
Of course it wasn’t the same as a personal visit, he knew that. He did miss the human touch, the familiar sense of companionship. And yet, this remote connection was also a strange comfort.
It allowed Mr Brown to remain independent, to hold onto his dignity, perhaps a small defiance against the ravages of time and inevitable loneliness that comes with it. The virtual visit ended, the blues and whites blinking out, leaving behind a weary old man in the quiet of his family home, surrounded by his memories and fading photographs, and yet somehow a little less alone than he was before.
The value of remote care.
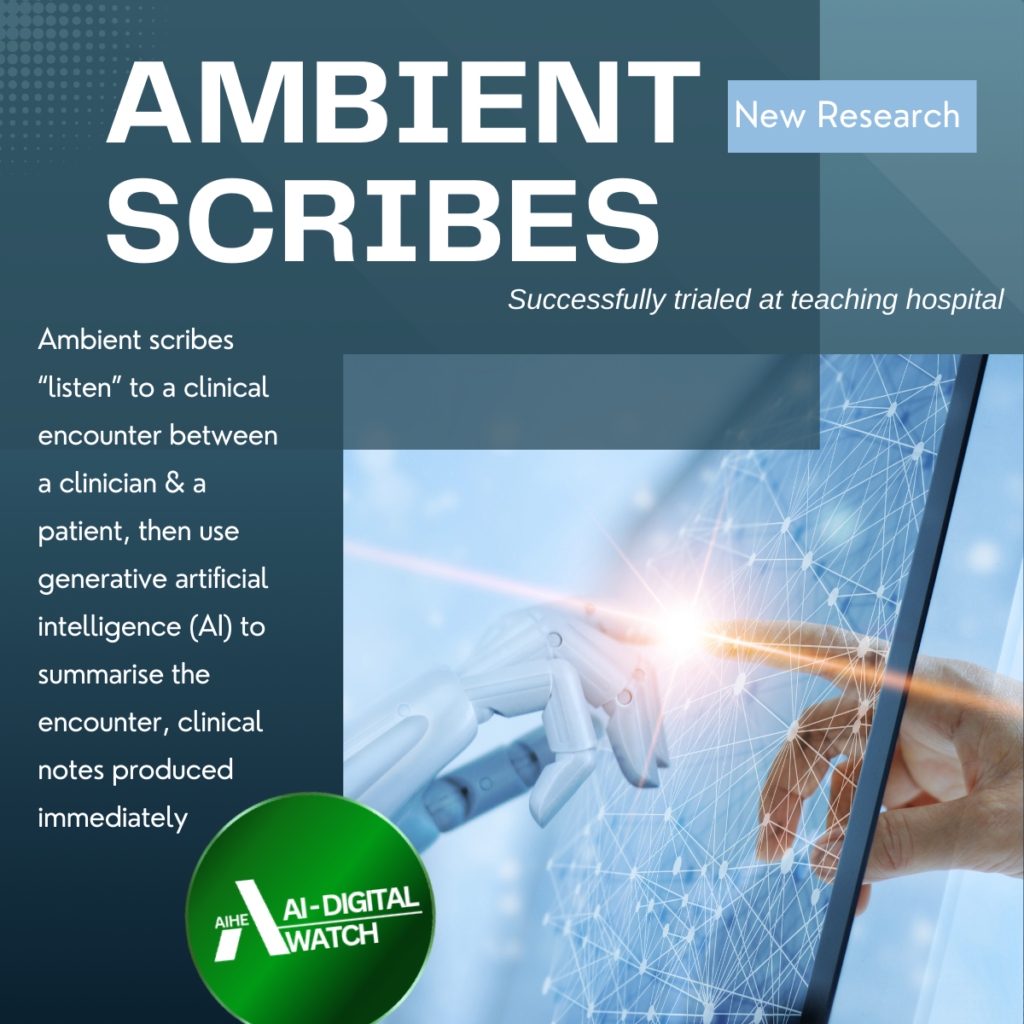
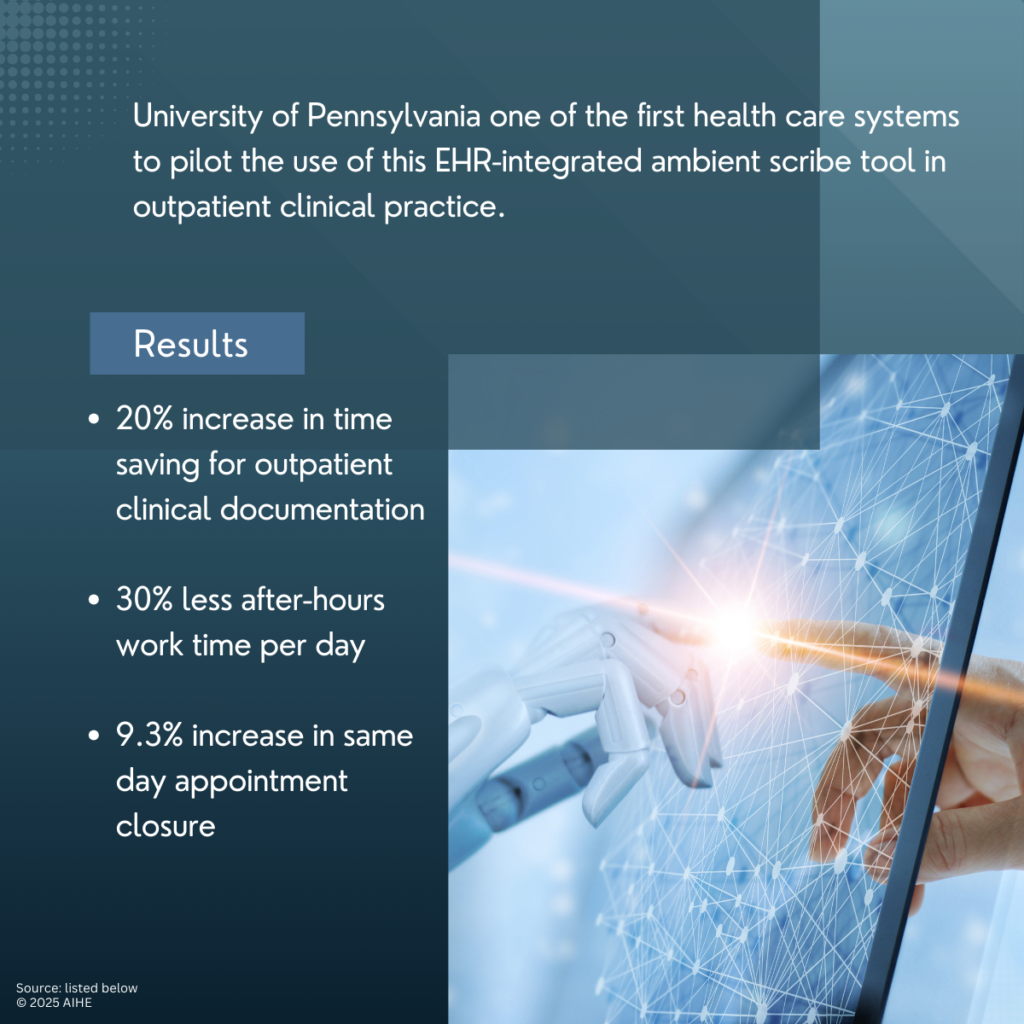
New research published last week, AI-driven ambient scribing technology has been found to successfully ease the burden of clinical documentation for healthcare providers, improving efficiency, reducing after-hours work and enhancing patient engagement.
The study, conducted by researchers at the University of Pennsylvania, examined the experiences of 46 clinician (physicians, nurse practitioners and physician assistants), across 17 specialties using an AI-powered ambient scribe integrated with Epic’s EHR system.
The tool captures patient-clinician conversations and automatically generates clinical notes, reducing the need for manual documentation.
Key findings:
Time spent on clinical notes decreased from 10.3 minutes per appointment to 8.2 minutes, on average.
After-hours work dropped from 50.6 minutes to 35.4 minutes per workday for those using the tool.
Clinicians reported lower mental strain associated with documentation and an increased ability to focus on patient interactions
In 2025 the healthcare sector faces a trifecta of cybersecurity concerns. Understanding and mitigating for these will allows healthcare organisations maintain system and operational integrity, safeguard patient hashtag#data, and ensure uninterrupted delivery of safe and effective services.
3 mitigation strategies for ransomware attacks:
• Robust backup and recovery processes for critical data systems
• Endpoint protection solutions to prevent malware infections
• Network segmentation & firewall implementation to limit the spread of ransomware
3 mitigation strategies for third party vendor breaches:
• Ensuring vendors meet minimum security standards & comply with regulations
• End to end data encryption
• Restrictiom of access controls & privileges to essentials
3 mitigation strategies for legacy system data breaches:
• Virtual patching solutions for known vulnerabilities
• Segmentation of legacy system from rest of network
• Minimising the amount of sensitive data stored in legacy systems by migrating to more secure locations
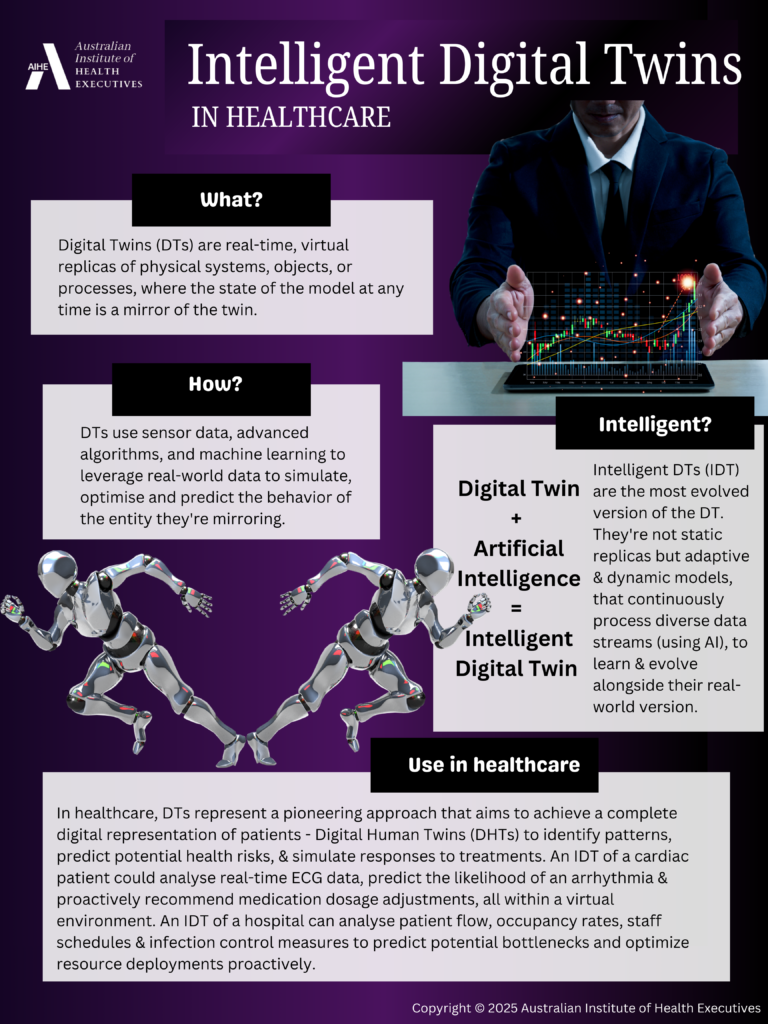
Move over AI, Intelligent Digital Twins (DTs) are rapidly emerging as a solid contender in the global healthcare transformative technology race.
Digital Twins (DTs) are real-time, virtual replicas of physical systems, objects, or processes, where the state of the model at any time is a mirror of the twin.
DTs integrate sensor data, advanced algorithms, and machine learning to simulate, monitor, and predict the behaviour of the physical entity they represent, creating the possibility for developing personalised representations of patients, medical devices, and even entire hospital systems.
Intelligent DTs are the most evolved version of the DT; a self-adaptive twin integrated with artificial intelligence, that has autonomy with learning, reasoning, knowledge, and acting capabilities, which can communicate with other twins.
This opens the path for unprecedented opportunities across healthcare as we know it, enabling personalised treatment analysis, enhancing medical device design and optimising hospital operations.
Imagine a cardiologist being able to minimise the risk of adverse reactions and maximise the therapeutic benefits of medications by simulating the impact of various combinations on a patient’s digital representation.
Or device manufacturers being able to simulate real-world usage scenarios on virtual prototypes to identify design flaws, optimise performance, and accelerate the device development process. Or creating virtual representations of entire healthcare facilities to mirror their workflows in real-time, to identify bottlenecks and predict surges to allow proactive resource allocation and utilisation.
In healthcare, these are some of the pioneering approaches being targeted by IDTs, and as this technology matures, it’s impact on healthcare can only be expected to grow.